Australians’ access to and views of psychological treatment for pain
As part of Psychology Week 2020 the APS and the Australian College of Applied Psychology produced The Australian Pain and Psychology Report 2020, based on a national survey of adults. The survey examined Australians’ experiences of chronic pain, access to psychological treatment among those with pain and attitudes towards psychological treatment among those with and without pain.
Survey overview
A representative sample of Australian adults (n = 1022) completed an online survey about their experiences with pain and their access to, and views of, psychological treatment for pain. The data was collected over a period of 2.5 weeks from 19 July to 6 August 2020, with assistance from an external market research agency, Pureprofile. Additional recruitment by the research partners also occurred but will be reported on separately.
Some key findings from the data about Australians’ access to and views of psychological treatment are summarised in this article.
Attitudes towards psychological treatment for pain
Willingness to try psychological treatment
People with and without pain within the last month were asked how willing they would be to try psychological treatment. Overall, 62 per cent of the sample indicated that they would be willing1 to try psychological treatment for a pain problem. Among those with pain, 65 per cent were willing to receive psychological treatment, which was significantly higher than the proportion of those without pain (45%) who would be willing to try psychological treatment if they were experiencing pain.
Views on the effectiveness of psychological treatment of pain
Half of the overall sample believed psychology would be moderately or extremely effective for helping someone who is experiencing pain. Those with pain within the last month viewed psychological treatment as significantly more effective than those without pain. In addition, those respondents who had seen a psychologist for pain viewed psychological treatment as significantly more effective than those who had not seen a psychologist.
Barriers to seeing a psychologist
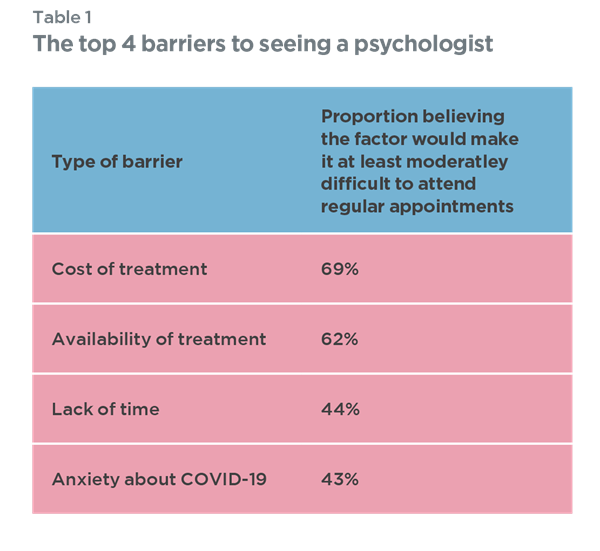
Australians with and without pain were asked about the degree of difficulty different factors would make it for them to see a psychologist regularly. The main barriers reported were concerns about the cost of psychological treatment and the availability of treatment both in terms of believing there to be a lack of treatment available and not knowing how to find a psychologist (see Table 1).
Table 1. The top 4 barriers to seeing a psychologist
Knowledge of and experience with psychological treatment
Awareness and experience of psychological treatment options for pain
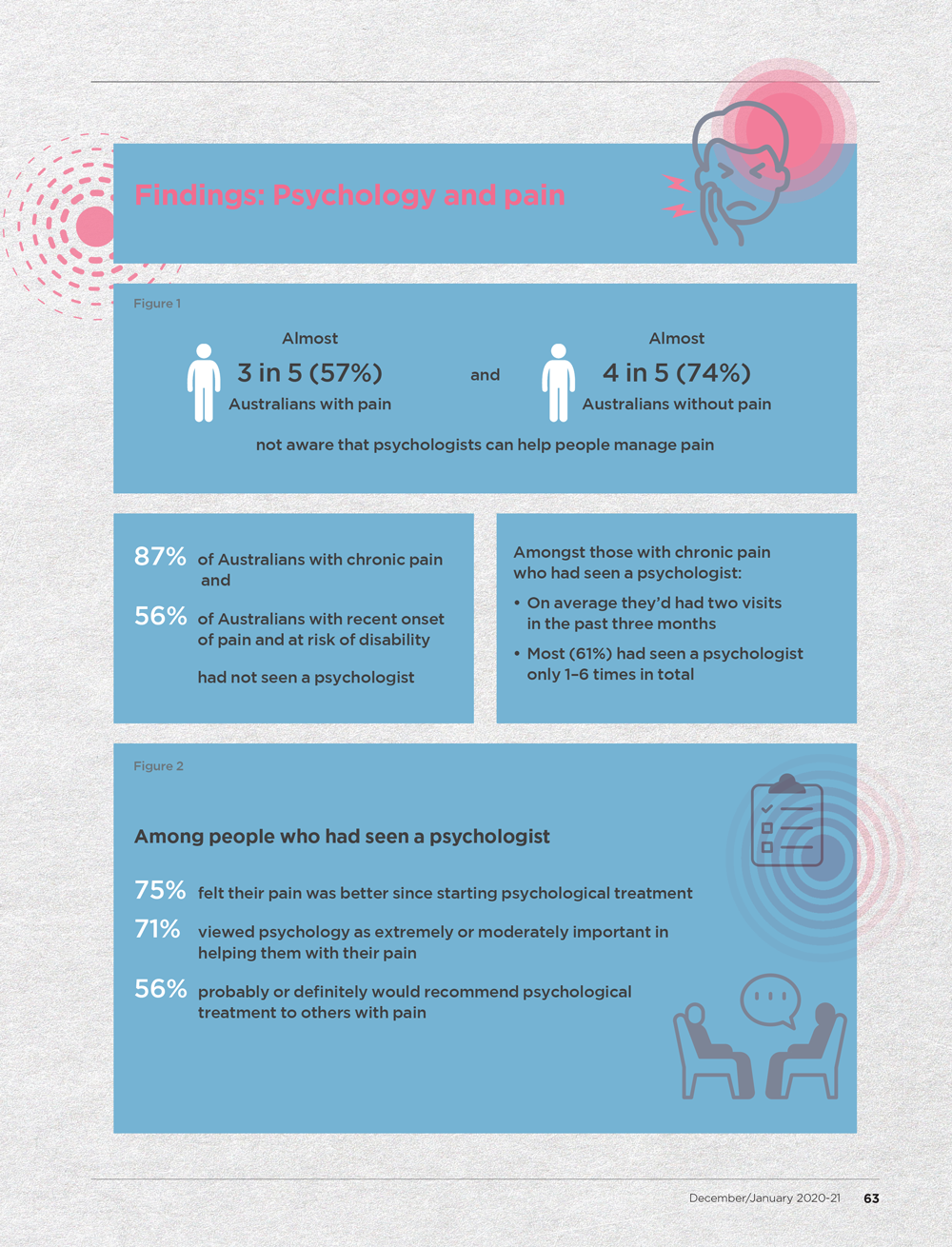
Australians with pain had limited awareness of, and experience with, psychological treatment options for pain (Figure 1). Fifty seven per cent indicated they were not aware that psychologists can help people manage pain, while 74 per cent of Australians without pain indicated that they were not aware that psychologists can help people manage pain.
Only 13 per cent of Australians with chronic pain 2 had seen a psychologist. Among those with chronic pain who had seen a psychologist, on average they had seen a psychologist twice in the last three months. Most (61%) had seen a psychologist one to six times in total.
Importance of psychological treatment of pain
Most Australians who had seen a psychologist for pain viewed psychological treatment as an important part of recovery (see Figure 2). People who had seven or more sessions with a psychologist rated the importance of psychology and their improvement as significantly greater than people who had six or fewer sessions.
Survey implications
Most Australians who had seen a psychologist for a pain problem viewed psychological treatment as an important part of recovery. However, in general, Australians with pain had limited awareness of and experience with psychological treatment options for pain. Among those Australians in the current study with chronic pain, only 13 per cent had seen a psychologist and most (61%) had done so fewer than seven times. Research suggests that six sessions with a psychologist is generally insufficient for treatment gains for chronic pain, except in mild cases (Guzman et al., 2001).
The number of sessions needed is variable but many individual client programs involve up to 10 sessions and some clients will need intensive programs of 100 plus hours (across all disciplines) (Agency for Clinical Innovation, 2015). The current survey findings suggest that many Australians with pain who would benefit from psychological treatment are either not getting it at all or may not be receiving a sufficient number of sessions for recovery.
Common barriers to seeing a psychologist were concerns about the cost of treatment and perceived lack of available services. Concerns about the cost of treatment are understandable given that most of the participants did not have funding for treatment via a compensation scheme and given limited Medicare funding specifically for psychological treatment of chronic pain.
Ways of increasing access to psychologists need to be considered, such as advocating for chronic pain specific Medicare items. The APS has called on Government and stakeholders to take action (bit.ly/3pXpgIo).
There is a need for further promotion in the community and with general practitioners and other allied health professionals and health services of the role of psychologists and psychological treatment in pain management, including increasing awareness of how psychologists can help and increasing knowledge of how to access a psychologist. This was the aim of Psychology Week 2020. The APS has developed three information sheets for the public about pain and how psychology can help (bit.ly/3q0TJ8D).
The APS has also developed resources for members on working with chronic pain in adults, including developing an online module (bit.ly/3l2YavR) and a practice guide (bit.ly/375qTen).
The full report of the survey is available from the Psychology Week campaign website: psychweek.org.au