There are myriad reasons why client-facing psychologists join the profession. To help people. To make a difference to the individual, as well as the community. To be part of something bigger than themselves. Holding on to that purpose can become challenging when the day-to-day demands that come with the role overshadow the outcomes. The juggle that comes with practice is real: the clients themselves, the ethical and legal requirements, administrative workload, Medicare... and on top of this, caseload management.
This last piece of the puzzle – caseload management – has become a big challenge for our members during the past 18 months. Not only have you been dealing with the professional impacts of the pandemic – the transition to telehealth, the intricacies of COVID-19 announcements and public health orders – but the demand for your services has shot up dramatically.
Dealing with unprecedented demand
We know that before the pandemic, one in four people were living with a mental health condition. This had already grown from one in 10, from years before. There are estimates that this has now blown out to one in two people, driven by the many and varied pandemic impacts: job losses, lockdowns, schooling from home, social restrictions.
This year we had heard anecdotally from members that this surge was resulting in burnout and expanding waitlist times, but we wanted to know more. We wanted to know the full extent of how COVID was affecting your ability to do the work you love – so that we can make it clear to governments what they can do to improve mental health systems around the country.
What we learned
In September, we surveyed our practising members and 1000 responded through the ThoughtExchange platform. By sharing your thoughts and rating others’, we quickly identified some clear findings:
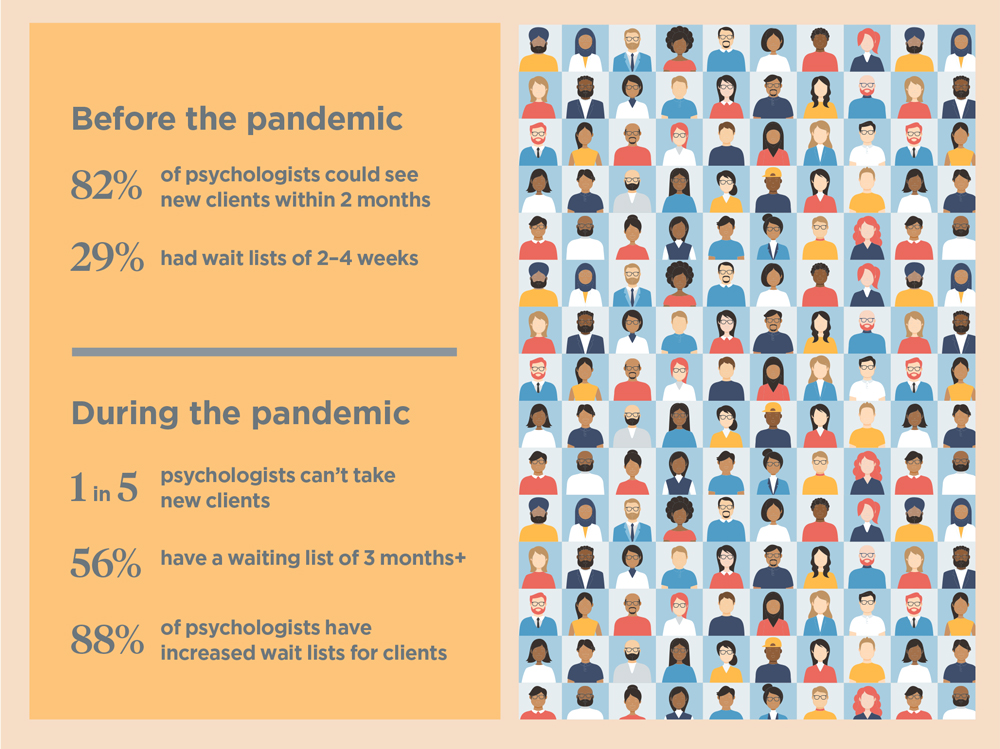
- 1 in 5 psychologists in Australia have had to close their books to new clients – a twentyfold increase on pre-pandemic figures
- 88 per cent of psychologists have seen an increase in wait times since March 2020, with 58 per cent reporting dramatically increased wait times
- 56 per cent currently have a waiting list of three months or more (or closed books) for new clients
- Prior to the pandemic, 82 per cent of psychologists were able to see a new client within two months, with 29 per cent reporting a wait list of just two to four weeks.
A twentyfold increase on psychologists closing their books since the pandemic cannot be overstated. The media has published many stories of how clients, who have gone through the process of getting a mental health care plan, are falling at the final hurdle just when they need help the most. This is not only affecting clients, but psychologists as well.
How this is impacting you
For psychologists, who ideally want to see everyone who needs help if clinically appropriate, this is incredibly difficult. Telling clients you can’t see them for three months goes against everything you committed to as a psychologist. But as a health professional, you have to ensure you’re providing the best possible care and giving your existing clients the care they deserve, too.
It’s not simply a case of taking on ‘just one more’ – you’re committing to that persons’ care, and if you don’t have availability to do so, it would be unethical to compromise that. That’s why it’s so important we have a plan and a pathway out of this situation – for clients and for psychologists.
What we are doing
There is a strong case for governments to build on these results and look closely at improving Australians’ ability to see a psychologist. At a time when policymakers are looking to us for solutions, our ability to speak as a collective is a real strength.
We know that people have long struggled to find the support they need and have been falling through the cracks of a complex and impenetrable mental health system. The Royal Commission into Victoria’s Mental Health System final report revealed this (bit.ly/2ZxBXl2).
We also know that we need to grow the workforce to meet the demand right into the future. The APS has been published widely in the media on this topic and we have been speaking to governments since the start of the pandemic, calling on the need for a dedicated national psychology workforce target with at least 20 per cent growth within three years (bit.ly/3auFnGQ).
We need to see trainee psychologists given permission to do more work across the public and private sector as a short-term solution to help meet the current surge in demand. Embracing technology to take the burden off the client and to make it easier for them to be matched to a psychologist through virtual waiting room technology is also a live option.
The fact that there has been record spending by state governments and the federal government on mental health is encouraging. The 2021 Federal Budget has committed funding to attract, upskill and redistribute mental health professionals. We will continue to engage with them on how this can be best spent.
Looking after yourself
As large parts of Australia track the course out of extended lockdowns, there will be relief for many. But this also spells the beginning of a very long road out for many people struggling with mental health challenges.
Taking the time to look after yourself is just as important as the time you are taking to look after your clients. Reaching out to one another for support and using our tools and resources, such as our free self-care course, are small but important steps to maintain the drive and capacity to continue doing the work you love (bit.ly/3mEGmtM).