The Australian Government's current health reform agenda provides a timely opportunity to highlight the contribution of health psychology interventions in the prevention and management of chronic diseases associated with lifestyle risk factors. The World Health Organisation (2009) has identified the main risk factors responsible for deaths internationally as high blood pressure (responsible for 13% of deaths), tobacco use (9%), high blood sugar (6%), physical inactivity (6%), overweight and obesity (5%), high cholesterol (5%), unsafe sex (4%) and alcohol use (4%). A number of these factors also increase the risk of major chronic diseases - cardiovascular disease, diabetes and cancers. There is now a substantial evidence base for the effectiveness of health improvement interventions based on psychological theory, research and practice and hence they deserve a high level of recognition within systems for funding health. This article presents a summary of a systematic review of the evidence for the effectiveness of health psychology interventions in the prevention and treatment of chronic diseases associated with lifestyle risk factors.
Review of the evidence base for health psychology interventions
The primary literature searching strategy for this overview was to identify systematic reviews published on the Cochrane collaboration website between 2001 and September 2009. The systematic review by Loxley et al. (2004) was also drawn upon in the summary of literature related to tobacco, alcohol and illicit drug interventions. In some cases other systematic reviews adopting similar standards to those adopted in the Cochrane reviews were also utilised.
In reviewing the evaluation literature against various health targets the distinction is made between treatment and prevention. In the present context treatment refers to interventions addressing populations already experiencing the health issue being addressed, while prevention efforts work with either the whole population or vulnerable sub-groups to reduce the risk of developing the targeted health outcome.
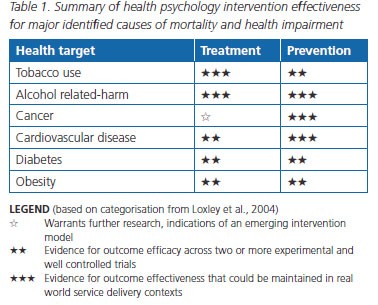
The evaluation evidence for health targets and effectiveness of interventions relevant to a number of the major identified causes of death and health impairment is presented in Table 1. A summary of the main conclusions of the review follows.
Tobacco use
Treatment
Over the past four decades psychological research and theory has played an important role in the development of interventions to help people quit smoking. In concert with a range of other strategies these interventions have assisted a large population who have negotiated the difficult behaviour change from smoking dependence to abstinence. Smoking rates in Australia have reduced from above 70 per cent fifty years ago to the current rates that are below 20 per cent. There is strong evidence for interventions in health settings where health professionals were encouraged to assess smoking behaviour and then deliver a brief intervention to encourage and advise on behaviour change. A number of treatment programs for dependent tobacco users were also found to have evidence for their effectiveness.
Prevention
There is strong research evidence that a number of strategies are effective in preventing tobacco use. Many of the important strategies rely on economic and legislative mechanisms such as tobacco taxation to create price disincentives and the enforcement of passive smoking regulations. However there is also efficacy evidence supporting the contribution of interventions that make use of psychological science, including drug education and social marketing strategies (Loxley et al., 2004).
Alcohol-related harm
Treatment
There is strong evidence that a number of strategies are effective in treating alcohol use disorders including substance abuse treatment and brief interventions, such as motivational interviewing, family/relationship interventions, relapse prevention, contingency management approaches and social skills training. Examples of effective brief intervention strategies include: surveying alcohol use at entry to university, community-wide health screening for symptoms of liver damage, and screening within a health care consultation.
Prevention
Many of the most effective strategies for preventing alcohol-related harm are based on economic and legislative principles including price controls (taxation), legislation and enforcement (e.g., minimum drinking age laws, public drunkenness laws) and market controls (e.g., liquor licensing, alcohol server training). Effective preventative interventions that have incorporated principles from the psychological sciences include random breath testing, school-based alcohol education and parent education (Loxley et al., 2004).
Cancer
Treatment
There is evidence from systematic reviews that exposure to psychological therapies improved treatment and disease-related symptoms for 14 per cent of adult cancer patients (Meyer & Mark, 1995). Psychological interventions also reduce psychological problems experienced by people with cancer.
Prevention
Behavioural interventions play an important role in reducing risk factors for cancer including the reduction of tobacco use and excessive alcohol use (see above).
Cardiovascular disease
Treatment
Jolliffe et al. (2000) demonstrated that the addition of exercise to existing heart care interventions reduced mortality by 27 per cent. A large review (Rees et al., 2004) concluded that psychological interventions (stress management and advice on risk factors) showed no effect on total or cardiac mortality, but showed small reductions in anxiety and depression for patients with chronic heart disease.
Prevention
Psychological and behavioural interventions have been demonstrated to play an important role in reducing risk factors for cardiovascular disease including the reduction of tobacco use, excessive alcohol use (see above), inactivity and depression.
Diabetes
Treatment
Within type 2 diabetes patients, Thomas et al. (2006) found exercise reduced physical symptoms and Norris et al. (2005a) found weight loss strategies were effective using dietary, physical activity or behavioural interventions.
Prevention
Nield et al. (2008) found that interventions providing dietary advice reduced diabetes symptoms. Norris et al. (2005b) found that weight loss interventions produced small significant weight reductions and also prevented diabetes in people with pre-diabetes symptoms.
Obesity
Treatment
Shaw et al. (2005) found that behavioural and cognitive behavioural interventions resulted in small significant reductions in overweight and obesity.
Prevention
Summerbell et al. (2005) found interventions designed to prevent obesity in childhood through diet, physical activity and/or lifestyle and social support resulted in improvements in diet and physical activity. Some studies that focused on dietary or physical activity approaches also showed small reductions in overweight and obesity.
Cost-effectiveness of psychological interventions
Systematic reviews have been conducted and indicate that well conducted psychological interventions have the capacity to achieve net savings in the health system and other tangible and intangible social costs.
Treatment
A meta-analysis of 91 studies published over the previous three decades (Chiles et al., 1999) examined the efficacy of psychological treatments on the cost of medical services. On average the savings in medical costs obtained through the implementation of psychological services was around 20 per cent. There is further evidence that psychosocial interventions can reduce costs in primary care, cancer treatment and alcohol abuse treatment settings.
Prevention
Economic evaluations have demonstrated clear net economic benefits with respect to a wide range of health and social costs through the delivery of prevention and early intervention programs based on behavioural and psychological knowledge targeting children and young people.
Conclusion
There is substantial evidence that health psychology interventions are effective in the prevention and treatment of lifestyle-related chronic diseases. Given that this is a major priority of the Australian Government's health reform agenda, psychologists are well placed to make a significant contribution to addressing the challenges of major health problems that are caused or exacerbated by lifestyle issues.
The author can be contacted at [email protected].
This article is based on a project undertaken over the last five years for the APS College of Health Psychologists to review and disseminate the evidence for the effectiveness of health improvement interventions (Toumbourou, 2010).